By Donald G. McNeil Jr.
Feb. 12, 2018
[Update: State financial regulators in New York said that they would investigate reports that gay men have been denied insurance policies covering life, disability or long-term care because they were taking PrEP.]
Three years ago, Dr. Philip J. Cheng, a urology resident at Harvard’s Brigham and Women’s Hospital, nicked himself while preparing an H.I.V.-positive patient for surgery.
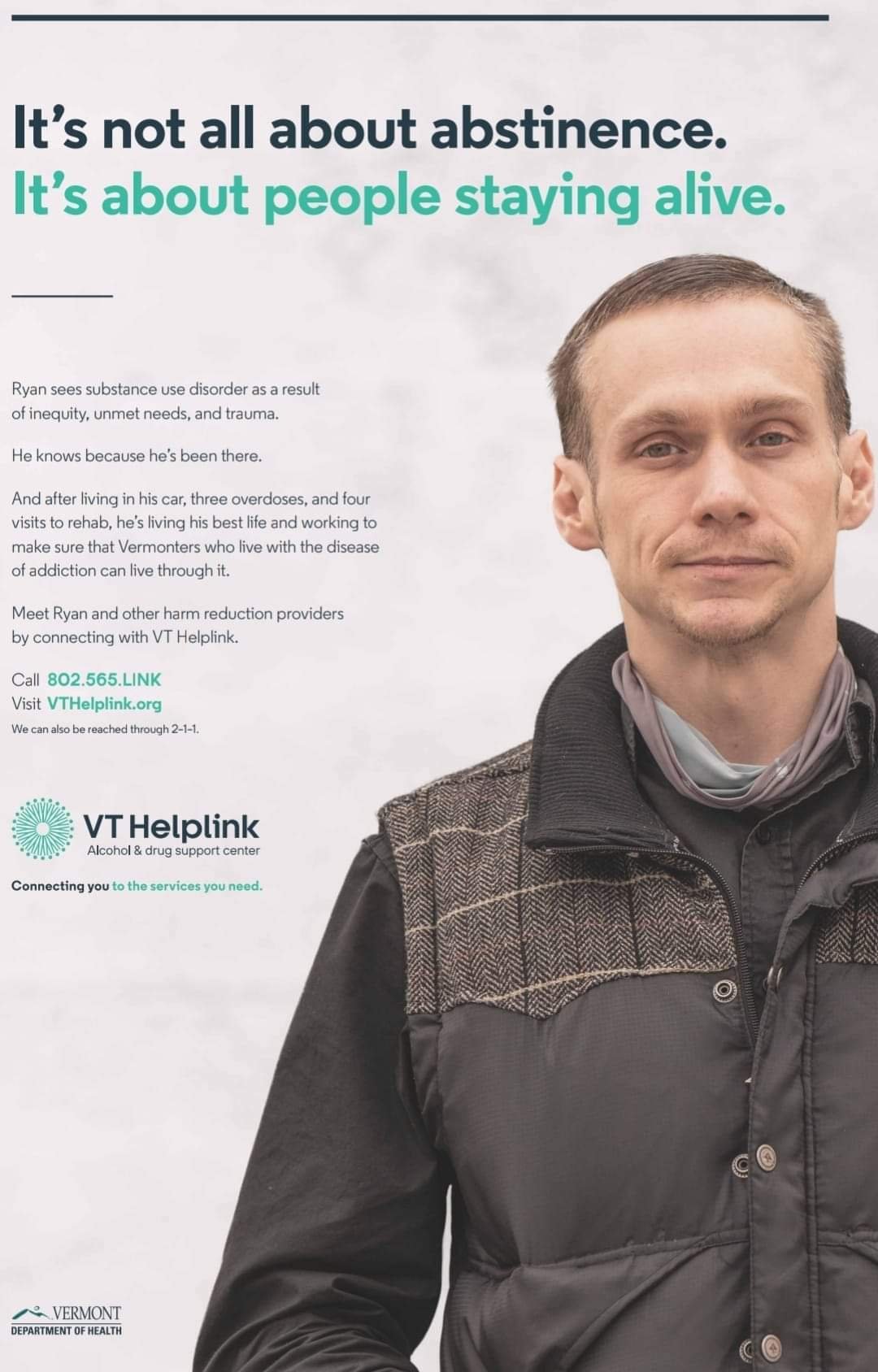
Following hospital protocol, he took a one-month course of Truvada, a cocktail of two anti-H.I.V. drugs, to prevent infection. Later, because he was an unattached gay man, he decided to keep taking Truvada to protect himself from getting H.I.V. through sex.
The practice — called PrEP, short for pre-exposure prophylaxis — is safe and highly effective. Several studies have shown that users who take the drug daily are at nearly zero risk of H.I.V. infection.
But when Dr. Cheng applied for disability insurance — which many young doctors do to protect a lifetime’s worth of income should they be hurt — he was told that, because he was taking Truvada, he could have only a five-year policy.
Dr. Cheng is healthy, has never had surgery or been hospitalized, and takes no other medication. “And I never engaged in sexually irresponsible behavior,” he said. “I’ve always been in longer-term monogamous relationships.”
“I was really shocked,” he added. “PrEP is the responsible thing to do. It’s the closest thing we have to an H.I.V. vaccine.”
Unable to get the company to change its decision — even after he offered to sign a waiver voiding his policy should he become H.I.V.-infected — he did what some other gay men in similar situations have been forced to do. He stopped taking Truvada.
He then applied to a different insurer — and was offered a lifetime disability policy.
There are nearly 800 life insurers in this country, according to the American Council of Life Insurers. There are no national figures on how many of them have denied coverage to men because they take PrEP.
But insurance brokers, gay-rights advocates and staff at medical clinics said in interviews they had heard of numerous such cases. H.I.V. specialists say the denials endanger men’s lives by encouraging them to drop PrEP if they need life, disability or long-term-care insurance.
By contrast, health insurance companies usually cover PrEP, which the Centers for Disease Control and Prevention endorsed in 2014 for anyone at substantial risk of H.I.V., which includes any gay or bisexual man who might have sex without a condom with anyone of unknown H.I.V. status.
The denials turn the insurance industry’s risk-management standard on its head: men who do not protect themselves can get policies, while men who do cannot.
“It doesn’t make any sense,” said Dr. Anthony S. Fauci, director of the National Institute of Allergy and Infectious Diseases, and perhaps the nation’s best-known AIDS doctor. “It ought to be the other way around.”
Dr. Robert M. Grant, the AIDS researcher at the University of California, San Francisco, who led the clinical trial that established the value of PrEP, said such denials “really are silly — it’s like refusing to insure someone because they use seatbelts.”
Moreover, advocates argue, the practice singles out gay men for discriminatory treatment. Women, for instance, are not denied coverage if they use birth control pills or get the vaccine against human papillomavirus, which can cause cervical cancer. Yet like Truvada, use of these drugs suggests an active sex life, with the accompanying risks.
And insurers routinely cover applicants with actual diseases controlled by medications, including diabetes, epilepsy, high blood pressure and bipolar disorder.
Bennett Klein, a lawyer for GLAD (GLBTQ Legal Advocates and Defenders), based in Boston, said he knew of 14 instances in which companies denied life insurance, long-term-care insurance or disability insurance to gay men on PrEP, or told brokers they would do so if asked.
Courtney Mulhern-Pearson, policy director for The San Francisco AIDS Foundation, said denial of life insurance to men on PrEP was “an increasing trend.”
When companies did offer explanations, they said applicants were turned down because the company believed they must be engaging in high-risk sexual behavior.
When she explained to some insurers that PrEP was protective, regardless of behavior, “there seemed to be an understanding,” she said. “But so far I haven’t seen any policy changes.”
Dr. Cheng’s stethoscope at home. He said his insurer claimed not to know about Truvada’s side effects, even though it was approved in 2004.CreditKayana Szymczak for The New York Times
The foundation considers the practice discriminatory, and Ms. Mulhern-Pearson has requested a meeting with California’s state insurance department “to see if there’s anything we can do legislatively or through regulation.”
The Times contacted the A.C.L.I., the industry’s trade association, and four of the companies named by Mr. Klein, sending each detailed questions about underwriting policies related to Truvada and the sexual habits of applicants, and what other medical conditions caused them to deny coverage.
An A.C.L.I. spokesman said the council did not collect such information from members.
For competitive reasons, companies do not publicize their underwriting standards and often do not explain why they deny an individual policy. Each policy is denied — or offered at a higher price or shorter term — based on many medical factors, including weight, blood pressure, cholesterol, smoking status and so on.
Mutual of Omaha, which Mr. Klein is suing for denying long-term-care insurance to an unnamed gay man, declined to answer any questions and said it did not comment on pending litigation.
In motions filed in GLAD’s suit, Mutual of Omaha conceded that it had denied an applicant coverage because he took Truvada.
The drug is indicated only for persons with H.I.V. or at high risk of acquiring H.I.V., the company said. Therefore it turned down everyone taking Truvada.
“The fact that the drug is less than 100 percent effective adds yet another layer to the risk profile,” the company added.
According to internal underwriting guidelines obtained by Mr. Klein, Mutual of Omaha sells long-term-care policies to people with Addison’s disease, bipolar disorder, depression, mild coronary artery disease, diabetes, epilepsy and high blood pressure, as long as they are controlled by medication for various periods, from six months up to three years.
It also insures former alcoholics who were alcohol-free and in support groups, as well as people who had recovered from heart valve surgery or cancers of the bladder, breast, prostate and skin.
“The irrationality is enough to make your mind spin,” Mr. Klein said.
Other insurers replied to The Times’s questions with brief answers saying they did not deny coverage solely for taking PrEP but declining to describe what conditions or behaviors would cause them to exclude coverage.
A spokesman for Lincoln National Life, in Fort Wayne, Ind., said it had approved policies for men on PrEP and had offered some lower rates reserved for low-risk clients. A spokesman was unsure when the company began doing so.
A spokeswoman for Principal National Life in Des Moines said the company “doesn’t decline individuals just because they’re taking Truvada” and did not quiz applicants about their sexual history. She declined to answer further questions.
A spokeswoman for Protective Life Insurance of Birmingham, Ala., said it “did not deny coverage based solely on Truvada use,” and might even offer a low-risk rate to someone taking the drug. She, too, declined to answer further questions.
Mr. Klein said he had sometimes heard similar answers from insurers even as men are denied coverage.
“I am fairly certain that this is just slippery language, and that they are excluding applicants when they see a diagnosis of ‘high risk sexual behavior’ or ‘exposure to H.I.V.’ in an applicant’s medical record.”
Those descriptions are linked to diagnostic codes that doctors use for reimbursement from health insurers when a patient asks for a prescription for Truvada. “That’s no different from excluding based on PrEP usage alone,” Mr. Klein argued.
Aaron E. Baldwin, a financial planner in San Francisco who specializes in clients living with H.I.V., said he had been seeing such denials for three years.
Some clients denied coverage, he said, were young executives with large student debts who wanted insurance so that should anything happen to them, their parents would not be saddled with payments.
In his experience, Mr. Baldwin said, companies in Midwestern and Southern states were reluctant to insure men taking Truvada, while Prudential, for example, insured even men with H.I.V. as long as they could show they took their medications every day.
In his case, Dr. Cheng said, a broker told him that the insurer claimed to be unsure about Truvada’s side effects. But the drug was approved by the Food and Drug Administration in 2004, and a study published in 2016 concluded that it was safer for long-term use than aspirin, which can cause gastrointestinal bleeding.
Dr. Cheng is now in a long-term relationship with an H.I.V.-negative man, and so he no longer takes Truvada. But the sting of his insurance denial lingers.
“It was blatant discrimination,” he said.
Correction: February 12, 2018
An earlier version of this article misstated the name of a company that provides insurance to men with H.I.V. It was Prudential, not New York Life.
Courtesy: The New York Times